胸腺增生是一种罕见的疾病。一般来说,它包括两种形态类型:真性胸腺增生(TTH)和淋巴滤泡增生。TTH显示胸腺增大,胸腺组织增加,而胸腺组织保持正常组织。TTH发生(1)作为一种免疫反弹现象(即.压力情况,类固醇的使用,库欣综合征或恶性肿瘤治疗后,(2)与内分泌异常有关(即Graves病、Addison病、结节病和Beckwith-Wiedeman综合征,或(3)以其最罕见的临床病理形式与其他疾病无关(特发性TTH)。TTH主要发生在新生儿、婴儿和较大的儿童,主要是由于学龄前胸腺功能的活跃。
Thymic hyperplasia is a rare disorder. In general, it embraces two morphological types: true thymic hyperplasia (TTH) and lymphofollicular hyperplasia. TTH indicates enlargement of the thymus gland by an increase in thymic tissue, which remains normally organized. TTH occurs (1) as an immunologic rebound phenomenon (i.e. stress situations, administration of steroids, following treatment of Cushingʼs syndrome or malignant tumors), (2) in association with endocrine abnormalities (i.e. Gravesʼ disease, Addison disease), sarcoidosis, and Beckwith-Wiedeman syndrome, or (3) in its rarest clinicopathologic form devoid of association with any other disease (idiopathic TTH). Mainly due to the active function of the thymus in pre-adults, the majority of TTH cases occurred in neonates, infants, and older children. We present the first case of idiopathic TTH in an adult, which was successfully resected via subxiphoid thymectomy.
TTH也可见于成人,与其他相关疾病无关。与免疫反弹TTH和疾病相关TTH相比,特发性TTH的主要治疗方法是根治性手术切除,可通过微创剑突下技术安全地进行。
TTH could also be found in adults irrespective of other associated diseases. In comparison to immunologic rebound TTH and disease-related TTH, the main treatment for idiopathic TTH is its radical surgical excision, which can be safely performed via minimal-invasive subxiphoid techniques.
https://www.thieme-connect.com/products/ejournals/html/10.1055/s-0039-1678254Thymic hyperplasia is a disorder whereby there is hyperplasia of the thymus gland.
Thymus hyperplasia can be subdivided into two forms:
lymphoid thymic hyperplasia
Both true thymic hyperplasia and lymphoid hyperplasia manifest as diffuse symmetric enlargement of the thymus so that it is difficult to distinguish between the two types on the basis of imaging findings alone.
It is important that radiologists be able to distinguish thymic hyperplasia from neoplasm, which tends to present as a focal mass.
True thymic hyperplasia associations include:
rebound hyperplasia to chemotherapy/steroids (see: thymic rebound hyperplasia)
radiation therapy
burns
other severe systemic stresses
Lymphoid hyperplasia
This is also known as lymphoid follicular thymic hyperplasia or autoimmune thymitis. Lymphoid hyperplasia associations include
systemic lupus erythematosus
rheumatoid arthritis
scleroderma
Graves disease
Radiographic features
Diffuse symmetric enlargement of the gland is the key morphologic feature of hyperplasia (neoplasm tends to manifest as a focal mass).
MRI
Chemical shift artefact may be useful in differentiating from other tumors:
chemical shift MRI depicts no decrease in signal intensity of thymic tumors, unlike the decreased signal intensity of thymic hyperplasia
this can be formally calculated using the chemical shift ratio (CSR)
Differentiating normal from hyperplastic thymus can be difficult and guidelines for making this distinction and verifying the presence of normal thymus include:
presence of a convex contour of the thymus beyond 19 years of age
presence of soft-tissue lobulation
presence of increased thymic thickness (should be ≤1.3 cm beyond age 20 years)
presence of a diagnosis associated with thymic enlargement or hyperplasia, e.g. Graves disease
Nuclear medicine
FDG PET is often performed in patients with malignancy; however, differentiation between thymic hyperplasia and thymic involvement by malignancy is difficult because the thymus demonstrates normal physiologic uptake.
Thymic Hyperplasia
Definition
Includes lesions characterized by either:
Increase in thymic size to a degree not expected for the patient's age and clinical condition
Influx of reactive B cells into an otherwise normal thymus
Alternate/Historical Names
Thymic hyperplasia
As defined in the literature, refers only to thymic lymphoid hyperplasia
The term is potentially vague and the more precise terminology below should be used
Diagnostic Criteria
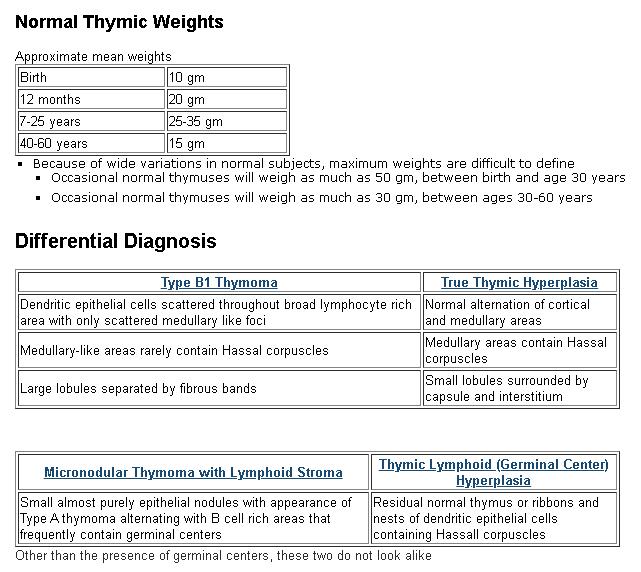
Thymic lymphoid hyperplasia
An more descriptive alternate term is thymic germinal center hyperplasia
Increased numbers of germinal centers
Predominantly in the interstitium and at corticomedullary junction
Occasional germinal centers may be seen in the normal thymus
No clear cutoff is defined
Residual thymus may be essentially normal in appearance or be distorted into ribbons and nests of epithelial cells
Usually does not lead to an abnormal thymic weight or size
Most frequently associated with myasthenia gravis
May be idiopathic or seen in other autoimmune disorders
Including sytemic lupus erythematosis, scleroderma and rheumatoid arthritis
Removal may improve myasthenia gravis symptoms
Germinal centers may also be associated with involvment of the thymus by neoplasms
True thymic hyperplasia
Thymus too big for patient's age
Under age 30, this means over 50 gm, see table
Histologically normal
Normal cortex, medulla, Hassal corpuscles and lobularity
No neoplasm
No reactive influx of cells
Cured by excision
Thymic rebound hyperplasia
Rapidly growing anterior mediastinal mass in a post chemotherapy patient
Some but not all cases exceed normal weight limits for age
Histologically normal
May be PET positive
Most often noted in lymphoma or germ cell tumor patients
Probably because the mediastinum is watched closely for recurrence of these neoplasms
Rapid growth and PET positivity may lead to surgical excision
Rebound hyperplasia itself is of no clinical significance
- Shimosato Y, Mukai K, Matsuno Y. Tumors of the Mediastinum, Atlas of Tumor Pathology, AFIP Fourth Series, Fascicle 11, 2010
- den Bakker MA, Oosterhuis JW. Tumours and tumour-like conditions of the thymus other than thymoma; a practical approach. Histopathology. 2009 Jan;54(1):69-89
- Bratton AB. The normal weight of the human thymus. J Pathol Bacteriol 1925;28:609
- Wekerle H. The thymus in myasthenia gravis. Ann N Y Acad Sci. 1993 Jun 21;681:47-55
- Mori T, Nomori H, Ikeda K, Kobayashi H, Iwatani K, Kobayashi T. The distribution of parenchyma, follicles, and lymphocyte subsets in thymus of patients with myasthenia gravis, with special reference to remission after thymectomy. J Thorac Cardiovasc Surg 2007;133:364-8